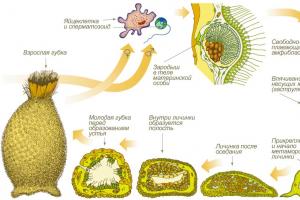
Artificial insemination, referred to by specialists as in vitro fertilization (IVF), is fertilization outside the body, i.e. in laboratory conditions or simply in vitro. Since the birth of the first “test tube baby” in 1978, artificial insemination has become one of the most important...
Infertility treatment
Indications for the use of donor sperm The husband’s sperm are completely absent due to a severe form of male infertility. In these cases, insemination with donor sperm is used. In some cases, if there are no sperm in the ejaculate, they can be obtained directly from the testicle using...
Infertility treatment
One of the main causes of infertility is a woman’s lack of ovulation - anovulation or very irregular ovulatory cycles - oligoovulation. In the natural cycle, in the area of the follicle that has ovulated, in a woman of reproductive age, the corpus luteum is determined, which prepares the endometrium...
Infertility treatment
Insemination is one of the methods of artificial insemination. Insemination with the husband’s sperm is recommended for infertility of unknown origin, with cervical factor immunological infertility in a woman, in the absence of “female factor”, but a slight decrease in sperm quality, with difficulties in carrying out...
Infertility treatment
In a number of chronic diseases of the female genital area, blood flow to the pelvic organs may be hampered due to changes in tissues and blood vessels. In this case, the medicinal effect is ineffective, since the medicinal substance does not reach the organ or tissue in the required volume through the bloodstream, often having a negative effect on the woman’s body as a whole. The combination of medication with physiotherapy can improve a woman’s condition with minimal medication.
Infertility treatment
When are donor eggs used? The use of donor eggs in an IVF cycle is due to the following medical indications, when the birth of a healthy child is impossible without the use of someone else’s genetic material: Lack of one’s own eggs or a sufficient number of them. Ovarian…
Infertility treatment
A surrogate mother is a woman whose pregnancy occurred in an IVF cycle after the transfer of an embryo with which she is not genetically related. In a surrogacy cycle, the eggs of an infertile woman are fertilized with her husband’s sperm and transferred to the surrogate mother’s uterus for subsequent gestation and…
Infertility treatment
Laparoscopy is a minimally invasive surgical operation that allows operations of varying degrees of complexity without incisions on the abdomen and scars that form after them. Such operations are carried out using special instruments inserted inside through small holes - punctures with a diameter of...
Infertility treatment
Ultrasound hysterosalpingoscopy (USGSS or EchoGSS) is an informative, non-invasive ultrasound examination of the uterus and patency of the fallopian tubes using vaginal and abdominal sensors. Diagnosis is carried out at a gynecologist's appointment in the first days after menstruation. The essence of the procedure...
Infertility treatment
Hysteroscopy is a surgical procedure in which a gynecologist uses a small, telescopic, lighted instrument (hysteroscope) to diagnose and treat abnormalities of the uterus. Using fiber optic technology, the hysteroscope transmits images of the cervical canal and uterine cavity to a monitor...
Infertility treatment
In most cases, qualified fertility doctors can determine the factors leading to infertility and prescribe appropriate treatment methods. Today, in the arsenal of reproductive specialists, andrologists, and urologists there are methods of treating infertility that provide a high chance of pregnancy and even a complete cure for infertility. Pregnancy occurs in more than 50% of patients who contact specialists in a timely manner.
Infertility Treatment Methods
- is this compatible?Treatment of female infertility
Treatment of endocrine infertility
At the initial stages of treatment, the normal functioning of the entire endocrine system is corrected: the thyroid gland, adrenal glands, and treatment of diabetes mellitus.
At the next stage, medications are used that stimulate follicle growth, then drugs that stimulate ovulation (the release of an egg from the follicle). All drugs to stimulate ovulation are selected by the doctor strictly individually. For more details, see section Endocrine infertility.
Tubal-peritoneal infertility
With help operative laparoscopy- microsurgical operation, obstruction of the fallopian tubes in both the isthmic and ampullary sections can be eliminated. Many gynecological operations were previously performed by major abdominal surgery (laparotomy). After laparoscopy (5-10 mm puncture), the likelihood of complications is much lower and patients recover much faster. In case of damaged fallopian tubes, infertility treatment using IVF is also possible. Often, even if it is possible to remove adhesions in the fallopian tubes, the ciliated epithelium lining the tubes from the inside may be damaged and not fulfill its role in moving the egg through the fallopian tube, which can threaten. Therefore, in case of severe tubal damage or in case of unsuccessful laparoscopy, IVF is the most preferred method of infertility treatment. For more details, see section Tubal obstruction.
Treatment of endometriosis
Drug treatment of endometriosis
The main principle of treating endometriosis with hormonal drugs is to suppress ovarian function and reduce excessive estrogen production. The hormonal drugs used lead to a state of temporary pseudomenopause and chronic anovulation - in which the growth of the endometrium and its monthly detachment do not occur, and the growth of endometrial tissue implants is also suppressed. For more details, see section Endometriosis.
However, the effect of hormonal therapy is temporary and, after its discontinuation, a relapse of the disease occurs.
Surgical methods for treating endometriosis
The effect of conservative treatment of endometriosis alone is not very high. Drug therapy can reduce pain symptoms and eliminate small areas of endometriosis. However, endometrioid cysts in the ovaries and adhesions cannot be removed by hormonal therapy.
With the help of laparoscopy, it is possible to remove foci of endometriosis, cysts, cut adhesions, while preserving the reproductive organs.
After the operation, painful symptoms decrease and pregnancy is often possible. In cases where surgery fails to remove all foci of endometriosis, postoperative therapy is performed. The most effective treatment is in 2 stages, leading to an increase in the effectiveness of treatment by 50%.
- Laparoscopy. The degree of spread, coagulation of foci of endometriosis, ovarian cysts, etc. are assessed.
- Hormonal therapy with GnRH agonists. Prescribed after laparoscopy to prevent and reduce relapse of the disease.
Some women with severe endometriosis experience such severe pain that they may need to have their uterus and ovaries removed to relieve the condition. Removal of the uterus is extremely rare and infertility treatment is usually carried out using more gentle methods.
Treatment of infertility in polycystic ovary syndrome (PCOS)
For polycystic ovary syndrome (PCOS), the initial stage of infertility treatment is weight loss(with excess weight) and, in the presence of carbohydrate metabolism disorders (insulin resistance), taking the drug Metformin. This drug increases the use of glucose in body tissues, normalizing its level in the blood, and also reduces appetite and helps regulate the menstrual cycle in women with polycystic ovary syndrome. Metformin doses are individual and determined by the attending physician. The duration of treatment is from 3 to 6 months. For more details, see section Polycystic ovary syndrome.
If such treatment is insufficient, ovulation is stimulated with Clomiphene citrate, which promotes the release of the egg from the ovary. Doses of Clomiphene citrate are determined individually. In the absence of ovulation, the dose of the medicine is increased.
At the same time, ovulation is monitored by measuring basal temperature and ultrasound diagnostics.
To stimulate the release of an egg from the ovary, the drug Chorionic Gonadotropin (Pregnil, etc.) is used. The effectiveness of treatment is determined by the presence of ovulation.
If treatment with Clomiphene citrate is insufficiently effective for 3 months, other medications are prescribed: Human menopausal gonadotropin (Puregon, Gonal-F). Treatment regimens are determined by the doctor individually.
Women with polycystic ovary syndrome who want to get pregnant are also prescribed progesterone in the second phase of the cycle, the dosage is determined by the doctor. At the same time, regular menstruation is restored, uterine bleeding and excessive growth of the endometrium inside the uterus stop. However, progesterone does not help cleanse the skin.
Surgical treatment of polycystic ovary syndrome
Surgical treatment of polycystic ovaries is used when ovulation cannot be achieved with medicinal methods. The main methods of surgical treatment of infertility in polycystic ovary syndrome are: wedge resection of the ovaries and electrocautery of the ovaries.
Wedge resection of the ovaries is an operation that is performed using a laparoscope (through small incisions in the abdomen) under general anesthesia. This involves removing a section of ovarian tissue that produces excess hormones. Reducing excessive hormone production after surgery helps normalize the menstrual cycle, promote ovulation, and make pregnancy possible. However, such surgical intervention in the future can lead to negative consequences for the reproductive system, causing the formation of adhesions and a decrease in the follicular reserve of the ovaries.
Electrocautery of the ovaries is a laparoscopic operation performed under general anesthesia. During electrocautery, a special instrument produces a targeted destruction of the part of the ovary that produces excess hormones.
As a rule, surgical treatment of polycystic ovary syndrome leads to the possibility of conceiving a child within the next 6-12 months.
Also an effective method of treating infertility in PCOS is in vitro fertilization.
Pathologies of the uterus
The main method of examination and treatment of pathology of the uterine cavity is currently hysteroscopy(examination of the uterine cavity using an optical device inserted into the uterine cavity through the cervix). Diagnostic or office hysteroscopy helps make a diagnosis. Diagnostic hysteroscopy uses a small diameter hysteroscope (about 3 mm) and does not require anesthesia.
At surgical hysteroscopy adhesions (synechias) are removed, septums are dissected, uterine fibroids and polyps are removed.
Depending on the size of the myomatous node, hormonal treatment and then surgery are first performed to reduce it. GnRH agonists are often used to treat patients with uterine fibroids and infertility in the preoperative period. Usually, after removal of fibroids, the ability to conceive is restored, but often after removal of fibroids, relapses occur, requiring repeated surgery.
In addition to endoscopic treatment methods, hormonal and anti-inflammatory drugs can be prescribed for diseases of the uterus. For more details, see section Pathologies of the uterus.
If pregnancy does not occur within two years after restoration of the normal anatomy of the uterus, doctors recommend IVF, including using surrogate mother.
Immunological infertility
Method of treatment cervical factor infertility is intrauterine insemination, in which the most motile sperm are separated from the seminal fluid and introduced through a catheter directly into the uterus, bypassing the cervical canal.
At antiphospholipid syndrome(AFS) microthrombi form in the circulatory system between the fetus and the mother, which leads to thrombosis of the placenta, a significant deterioration in fetal nutrition and early miscarriage. Treatment for APS is with low-dose aspirin, low-molecular-weight heparin, or steroids, which suppress the immune system's abnormal response.
In case of an immunological disorder, when the mother’s body rejects the fetus as “foreign”, which leads to early miscarriages, treatment methods include increasing the sensitivity of the mother’s body to the paternal genes by subcutaneously injecting his lymphocytes even before pregnancy. The basis for this is the assumption that the introduction of foreign cells stimulates the maternal immune system to initiate a normal immune response during pregnancy. Another treatment is the intravenous administration of immunoglobulin, a mixture of proteins obtained from the plasma of many donors to stimulate the mother's body to respond properly. For more details, see section Immunological infertility.
Treatment of infertility of unknown origin
Treatment options for patients with unexplained infertility include:
- wait-and-see strategy (do not undertake any fertility treatment and continue trying to conceive naturally);
- intrauterine insemination (IUI);
- stimulation of ovulation with clomiphene citrate (in combination with intrauterine insemination);
- stimulation with gonadotropins (HMG or FSH drugs) in combination with intrauterine insemination (HMG/FSH/IUI);
- in vitro fertilization (IVF) and micromanipulation of spermatozoa (ICSI) in combination with artificial rupture of the embryo membrane in vitro (assisted hatching).
Treatment of male infertility
Treatment regimen male infertility depends on the form, stage of the disease, underlying causes, as well as individual tolerance to various drugs. Only comprehensive and well-chosen treatment tactics under the supervision of a doctor lead to a positive result.
There are a variety of causes of male infertility, ranging from impaired development of the reproductive organs to environmental influences. The capabilities of modern medicine make it possible in most cases to accurately identify the cause and choose the optimal method of treating infertility.
Treatment for male infertility may include hormonal therapy to improve sperm maturation, antibiotic therapy for infections, surgical treatment of varicoceles, hypospadias, and injection of specially treated sperm into the woman's uterus ( insemination), in vitro fertilization () together with intracytoplasmic injection of sperm into the egg (), genetic analysis and other reproductive technologies for the treatment of infertility. For more details, see section
If a married couple cannot have a child after actively trying to conceive for a year, then in this case we can talk about infertility - female, male or combined. But most often, drug treatment for infertility is still prescribed for female infertility, when the patient is diagnosed with anovulation, that is, lack of ovulation.
Anovulation is a physiological or pathological condition of the reproductive system of the female body, in which the egg does not mature in the follicle and is subsequently released from the ovary, which means conception itself becomes impossible. Moreover, it is considered the norm in cases where a woman is pregnant, in the postpartum period (up to six months) or has already reached an age when the decline of the reproductive system is a natural process, that is, with the onset of menopause. However, if a woman is of reproductive age, then her lack of ovulation is regarded as a pathology. And the doctor prescribes drug treatment for infertility.
What could be the causes of infertility?
The state of anovulation is dictated by the fact that for some reason the interaction between the hypothalamus and pituitary gland is disrupted. That’s why the first thing the doctor pays attention to is the normalization of the functioning of the hypothalamus and pituitary gland. And only after this phase of drug treatment for infertility will it be possible to move on to the second - stimulation of ovulation. But first things first.
The hypothalamus is a part of the brain that controls the pituitary gland (gland). It in turn produces all the major reproductive hormones, such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH). And these hormones affect the functioning of the ovaries, which occurs cyclically, thus creating a woman’s menstrual cycle.
But the reasons that lead to the fact that the coordinated work of the hypothalamus, pituitary gland and ovaries is disrupted can be different, for example, the lack of ovulation occurs as a complication after long-term use of contraceptive drugs.
All sorts of diseases are becoming an indisputable risk factor: gynecological, endocrine, and so on, right up to brain injuries. Moreover, anovulation may not be associated with diseases, but may appear as a consequence of external influences such as stress or excessive physical exertion. Failures in the reproductive system also arise due to strict dietary restrictions, with which the body was not previously familiar, and which lead to rapid weight loss in record time.
Here is the most complete list of reasons:
- abortion;
- sharp increase/decrease in body weight;
- external influencing factors: stress, overwork, physical and psychological stress that a woman has not previously encountered in her daily life;
- neuroinfections, that is, infections that affect parts of the brain, such as meningitis and encephalitis caused by viruses and bacteria;
- violation of the norms for the number of follicles in the ovaries;
- hormonal imbalances: changes in the ratio of the production of certain hormones that affect the reproductive system;
- gynecological diseases: fibroids, endometriosis, chronic inflammatory processes of the genital organs, previous infectious diseases;
- endocrine diseases: polycystic ovary syndrome (PCOS), hyperprolactinemia (a condition in which the level of the hormone prolactin in the blood is higher than the permissible norm) and others. Endocrine diseases negatively affect the reproductive system, interfering with the process of preparing the female body for conception at all stages from the moment of follicle maturation to the preparation of the endometrium for further implantation of the embryo.
By the way, the detected polycystic ovary syndrome may not at all be a mandatory criterion indicating that the patient has been diagnosed with polycystic ovary syndrome. Even among specialists, there are those who mistakenly believe that these are synonyms of the same disease. But that's not true. So, in the case of polycystic disease, the main symptom indicating it will be anovulation, and in case of polycystic ovary syndrome, in addition to it, hyperandrogenism will be detected.
Hyperandrogenism is a condition of the female body in which excessive amounts of male hormones are produced; It can manifest itself in the form of acne, seborrhea, alopecia (baldness) or, on the contrary, hirsutism (increased hair growth).
At the same time, the doctor’s diagnosis of “polycystic ovary syndrome” excludes other diseases, such as congenital adrenal hyperplasia, tumor of the ovaries or adrenal glands that synthesize androgens, Cushing’s syndrome, hypothyroidism and the above-mentioned hyperprolactinemia.
Diagnosis and subsequent drug treatment of infertility
Unfortunately, it is not always possible to understand that difficulties with conception are caused by a lack of ovulation on your own, since a woman’s menstruation often continues and proceeds without interruptions. Thus, there are no symptoms that could indicate an existing problem.
If the menstrual cycle is disrupted (delays occur or periods stop altogether), then this is a reason to immediately consult a doctor.
Urinary rapid test
The simplest and most accessible method for diagnosing anovulation is a rapid urinary test. It is similar to a pregnancy test - it is aimed at detecting a specific hormone, in this case luteinizing hormone (LH), and is performed at home. The level of LH in the urine increases sharply when the follicle ruptures, which indicates the onset of ovulation in a woman. True, there is also a significant drawback - the rapid test is not one hundred percent reliable, since the LH level may increase for other reasons. For example, it can grow in cases of kidney dysfunction, as well as various endocrine and gynecological diseases, such as ovarian wasting syndrome and the like.
Thus, this test is only a primary diagnosis, after which the woman needs to see a doctor and undergo all mandatory tests and examinations. At the same time, there are many of them, because further drug treatment of infertility, which will be aimed at stimulating ovulation, is quite serious.
First of all, an ultrasound examination is carried out, which, due to its clarity, is considered the most reliable diagnostic method. It is prescribed on different days of the menstrual cycle so that it is possible to track the process of folliculogenesis (follicle development) at all stages. An ultrasound of the ovaries shows whether the process of egg maturation has started, and a repeat examination, which is usually carried out a few days later, shows whether ovulation occurred or not.
Blood for hormones
The analysis is carried out several times, since the level of hormones in the female body is not constant and can be different, and it is impossible to understand from just one control fence what is normal for a woman and what can be considered just a malfunction.

- follicle-stimulating hormone (FSH), based on its indicator, one can estimate the ovarian reserve of the ovaries, that is, the supply of follicles capable of developing, becoming dominant, and therefore capable of completing their development with ovulation. It is the level of FSH that the doctor will focus on in the future when prescribing drug treatment for infertility. The developed treatment regimen will depend on it - the most effective drugs in each individual case, as well as their dosage, will be selected. When the patient is over 35 years old, additional studies are prescribed to assess the ovarian reserve - tests are performed using various substances, such as clostilbegit and follicle-stimulating hormone analogues in order to predict what the ovarian response to stimulation will be.
- luteinizing hormone (LH), as a rule, is given simultaneously with FSH, and, along with it, is considered decisive for the normal functioning of the woman’s reproductive system. Reaching a peak, LH initiates ovulation, in addition, after the release of the egg, it starts the process of luteinization, the essence of which is to prepare the endometrium for possible implantation of the embryo. In this case, a low or high LH level indicates a certain type of anovulatory infertility. LH levels also influence the choice of drug treatment for infertility, which will be prescribed in the future by a fertility specialist. If the LH level is below normal, then drugs containing only FSH will be contraindicated. LH is also responsible for the production of progesterone (the female sex hormone), which is considered one of the main hormones during pregnancy, and its low content threatens to lead to abortion in the early stages.
- Prolactin is a hormone that is also called the “lactation hormone”, as it affects milk production in pregnant and lactating mothers. However, if it deviates from the norm, it can become the main cause of female infertility. It is able to suppress the formation of another hormone - follicle-stimulating hormone, and therefore prevent the onset of ovulation. When the level of the hormone prolactin is regularly higher than normal, then most likely we are talking about a disease - hyperprolactenemia.
- estradiol - refers to estrogens, which, in turn, are considered the main female sex hormones and play as important a role as testosterone for the male body. Estradiol is formed in the ovaries and is designed to prepare the female body for conception, including the uterine mucosa. Its deficiency is as important as an excess of prolactin and leads to infertility.
- androgens, male hormones such as testosterone and DHEA sulfate should be produced in small quantities by a woman, but their excessive levels in the blood negatively affect ovulation.
- Thyroid hormones (TSH, T3, T4) can also affect the growth of follicles, which means that if they deviate from the norm, they can interfere with conception.
Diagnosis of tubal patency and spermogram
If a gynecological disease such as obstruction of the fallopian tubes is detected, ovulation stimulation is not prescribed, since it will simply be ineffective, but spermogram indicators may indicate the need for procedures such as IVF or artificial insemination.
Other research and tests
Among the examinations that may be prescribed additionally are a test for the compatibility of spouses, an assessment of the ovarian reserve, which is especially important when the patient has already reached adulthood, a smear for sexually transmitted infections and oncocytology, and so on - everything will depend on the specific clinical situation.
Thus, before prescribing drug treatment for infertility, the reproductive specialist makes sure at the preparatory stage that the patient does not have concomitant diseases that can be regarded as contraindications to treatment, and there are no hormonal imbalances. After that, the specialist, based on the results of the studies, selects the most effective drug therapy regimen.
Patients who are encountering this problem for the first time may be prescribed more conservative treatment, which consists of taking birth control pills for a period of three to six months. During this time, the woman’s reproductive system should rest and her hormonal levels should recover.
Drugs can also be prescribed, provided that she does not have any endocrine disorders containing synthetic progesterone, which will suppress the process of follicle maturation, which again will lead to the fact that during their administration the pituitary-ovarian system will have time to rest.
Such medicinal methods, as a rule, are effective in cases where anovulation occurs due to external factors or as a complication after an illness. Again, their effectiveness will depend on the woman’s age. If such treatment methods still do not lead to the desired result, then the next step is to stimulate ovulation.
The first stage of treatment is aimed at normalizing the function of the hypothalamic-pituitary-ovarian system, and only after that the next stage is started, when ovulation is stimulated to achieve pregnancy. Traditional drug treatment for infertility is carried out with clostilbegit or gonadotropins; there is also a third option when the drugs are combined.
Treatment is carried out according to a specific scheme and exclusively under the supervision of a doctor.
Medicines for the treatment of infertility
Clostilbegit is a drug that is an artificially created analogue of natural estrogen, which stimulates the functioning of hormones such as FSH, LH and prolactin. Its uniqueness lies in the fact that when the content of estrogen in the body is low, it exhibits an estrogenic effect, and, conversely, when it is high, it performs the function of an anti-estrogen, that is, it has a bilateral effect. Moreover, its activity significantly exceeds the natural hormone.
The regimen for taking clostilbegit is strictly individual. If a woman has a regular menstrual cycle, then taking it begins on the 3rd or 5th day of the cycle; if there are no periods, then the day you start taking it does not matter, and with anovulatory infertility, everything will depend on the sensitivity of the ovaries to the components of the drug.
You should start taking it with small doses, and with each subsequent course (if necessary), the dosage increases, but it cannot exceed 750 mg during one cycle.
The instructions for this drug say that you can take it no more than five to six times in your life, since excessive use can lead to early depletion of the ovaries, which will lead to early menopause. So, after several courses that did not lead to the expected result, the treatment method should be reconsidered. Among the special instructions for taking this medicine is its negative effect on the endometrium, that is, if the endometrium is obviously thin, it is recommended to turn to other treatment regimens.
The second drug regimen that a doctor can prescribe is stimulation of ovulation through injections of gonadotropins, which are considered drugs of the so-called “new generation”. Two types of gonadotropins are used - menopausal and recombinant. The first is used when a more gentle effect on the ovaries is necessary. The second is considered the most “clean”, which affects its cost. Gonadotropins have a follicle-stimulating effect, increase the concentration of sex hormones, increase the concentration of estrogen, stimulate the growth of the ovaries, as well as the maturation of follicles in them and further ovulation.
A combined treatment regimen is also used, which allows to reduce the total dose of gonadotropins, as well as make treatment more affordable from a financial point of view.
An injection of hCG (human chorionic gonadotropin) is prescribed regardless of which drug was chosen for stimulation; necessary to start the ovulation process and also prevents the formation of follicular cysts.

During the period of drug treatment for infertility, it is necessary to regularly measure basal temperature (the lowest body temperature that is reached during dreams and is usually measured from the very early morning, when physical activity has not yet begun), as well as ultrasound to monitor the response of the ovaries to the therapy.
After ovulation occurs, so-called maintenance therapy is prescribed, which is based on medications containing the hormone progesterone.
In many cases, drug treatment for infertility leads to ovulation and the onset of a long-awaited pregnancy, but in some women, the use of drugs, like surgery, unfortunately does not give the desired result. Then the attending physician advises turning to assisted reproductive technology such as IVF.
Treatment specialists, doctors:
IVF (IVF) - 118,000 rub.
Procedure
Counter. stimulation
33,500P
General anesthesia
4 500 P
Puncture foul., first.
12 200 P
Fertilization IVF method
10,500 P
Cultivation
38 300 P
Embryo transfer
19,000P
IVF + ICSI (ICSI) - 145,000 rub.
Expand to view a list of services and costs
Procedure
Counter. stimulation
33,500P
General anesthesia
4 500 P
Puncture foul., first.
12 200 P
IVF Fertilization
10,500 P
Fertilization using ICSI method
27,000P
Cultivation
38 300 P
Embryo transfer
19,000P
IVF in the natural cycle - RUB 58,600.
Expand to view a list of services and costs
Procedure
General anesthesia
4 500 P
Puncture foll. (cysts)
9,500P
Fertilization in the natural cycle
6 800 P
Cultivation in a natural cycle
Scientists estimate that every sixth couple faces the problem of infertility. It is believed that the inability to become pregnant after a year of regular (at least two to three times a week) sex without using contraception is a reason to consult a specialist. Problems with conception, as is known, can occur on the part of both partners. In this article we will talk about modern methods of treating female infertility.
Lack of pregnancy is not always infertility
There are many reasons that can prevent pregnancy. And it should be noted that not all of them indicate the presence of organic pathology. Thus, studies have shown that women exposed to regular stress factors experience greater difficulty conceiving compared to their peers living in conditions of psychological comfort.
Therefore, if you cannot get pregnant for a long time, first of all, it would not be amiss to ask yourself the question - how harmoniously organized is my own life?
A woman’s body is designed intelligently, and if the expectant mother does not sleep enough, does not eat properly and is very tired, then the conditions for bearing and giving birth to healthy offspring are unsuitable, which can lead to female infertility. Treatment in this case is a recommendation to make your life more comfortable and calm, then conception will occur by itself without any intervention from doctors.
Doctors have found that infertility is more likely to occur in women who smoke. Overweight (BMI>30), as well as underweight (BMI<19) также могут негативно сказаться на женской фертильности. В некоторых случаях бесплодие может быть обусловлено приемом определенных лекарственных препаратов или воздействием профессиональных вредностей. Обязательно сообщите своему гинекологу о препаратах, которые вы принимаете, поскольку некоторые из них могут способствовать бесплодию.
But it also happens that a woman eats regularly, leads a healthy lifestyle, gets enough rest, but is diagnosed with infertility. Let's try to figure out what problems in her body can prevent conception, and how modern medicine treats infertility. Modern infertility treatment depends on the cause of the inability to conceive. A gynecologist must first use a medical examination to find out what the cause is and then prescribe targeted infertility treatment.
Treatment of infertility due to hormonal disorders
The endocrine system plays a key role in regulating the reproductive sphere. The hypothalamus is a small region in the diencephalon, closely connected to the pituitary gland. Together they form the so-called hypothalamic-pituitary system - the central link in the endocrine regulation of the body. Any pathology of the hypothalamus or pituitary gland can affect a woman’s reproductive abilities and lead to infertility.
In some cases, diseases of the hypothalamic-pituitary system are a consequence of traumatic brain injury or tumor. If the doctor has reason to believe that this is the cause of infertility, he may suggest that the woman undergo an MRI procedure (it is harmless and painless), and also suggest a study of the level of hormones in the blood (with tumors it can be significantly increased). Detection of a tumor may be an indication for surgical treatment.
Treatment of infertility due to ovarian pathology
Another organ whose damage leads to infertility is the ovaries. In addition to the fact that they are a “storage” for maturing eggs, they also produce the most important reproductive hormones: estrogens, androgens and progesterone. Ovarian diseases (cysts, tumors), thus, in most cases lead to hormonal imbalance, against which pregnancy does not occur, despite all attempts made.
Diagnosis of ovarian diseases usually includes ultrasound examination. In some cases, laparoscopic surgery is indicated, during which pathological tumors are removed. The ovarian tissue obtained during such an intervention is sent for histological examination, based on the results of which the doctor selects the appropriate treatment (usually hormonal drugs are used). Correction of ovarian pathology in this case is the key to treating concomitant infertility.
Treatment of infertility due to thyroid pathology
The thyroid gland may seem like an organ that has nothing to do with infertility. However, this opinion is erroneous: excessive activity of the thyroid gland (hyperthyroidism), as well as reduced function (hypothyroidism) can directly affect a woman’s ability to conceive and bear a child. Women with hypofunction of the thyroid gland in many cases suffer from menstrual irregularities, even lack of ovulation. An analysis of the level of thyroid hormones (triiodothyronine and thyroxine) will clarify the diagnosis.
For hyperthyroidism, treatment is aimed at lowering the level of thyroid hormones in the blood. This can be achieved with the help of drugs that inhibit their synthesis or, in especially severe cases, a section of the thyroid gland is excised during surgery. In case of hypothyroidism, the use of iodine preparations may be indicated. Achieving optimal levels of thyroid hormones in this case leads to the resolution of this cause of infertility and conception.
Treatment of infertility due to pathology of the reproductive system
In some cases, the inability to become pregnant may be due to a disease of the uterus or fallopian tubes.
Pathology of the female reproductive system can be divided into congenital and acquired. Congenital anomalies include: developmental features (bicornuate uterus, uterine septa and synechiae). Acquired pathology includes scars after previous surgical interventions (in particular, abortions), benign tumors (fibroids), endometriosis (pathological growth of endometrioid tissue in the uterine cavity and beyond), endometrial hyperplasia.
To confirm or exclude the presence of the above pathological conditions in female infertility, the attending physician will first prescribe an ultrasound examination for the patient. In some cases, a biopsy or separate diagnostic curettage may be indicated, followed by histological examination of the resulting tissue samples.
Treatment of infertility with surgery
If the cause of infertility is a benign tumor or congenital developmental features (bicornuate uterus, intrauterine septum, synechiae), the woman may be indicated for surgical intervention aimed at eliminating them. Operations of this kind in most clinics are performed laparoscopically. The woman is put into medicated sleep, after which the doctor gains access to the abdominal cavity through several small punctures in the anterior abdominal wall. To minimize the risk of damage to internal organs, as well as to ensure good visualization of the surgical field, carbon dioxide is injected into the abdominal cavity. The image obtained using the endocamera is displayed on the monitor, which allows the operating team to monitor each stage of the operation. Also, the resulting image can be recorded on digital media. Using laparoscopic technology, a significant part of gynecological operations can be performed: removal of an ovarian cyst or benign neoplasm, endometriotic lesions. The operation is minimally invasive: there are practically no scars left after it, and recovery occurs within a few days.
Another cause of infertility may be obstruction of the fallopian tubes. Normally, it is along them that the fertilized egg reaches the uterine cavity, where it attaches. If the tubes are obstructed (most often this occurs as a result of adhesions), the egg cannot enter the uterus and infertility develops. To make sure that the fallopian tubes are passable, the doctor may prescribe the woman an x-ray using a contrast agent - metrosalpingography. This study is also used for suspected intrauterine polyps, neoplasms, and synechiae.
What does a fallopian tube patency test show?
The method consists of the following steps. The doctor dilates the vagina using a special speculum, after which a special catheter is inserted through the cervix into its cavity, with the help of which it is filled with a radiopaque substance. After this, using an X-ray machine, images are taken to evaluate the contours of the intrauterine cavity and the patency of the fallopian tubes. So, if there are polyps or synechiae in the uterine cavity, they will appear on the image as a so-called filling defect. As for the fallopian tubes, if they are normal, the x-ray will show the flow of contrast into the abdominal cavity. If on one side the X-ray does not show the flow of contrast into the abdominal cavity, we can talk about obstruction of the corresponding fallopian tube.
How is infertility treated due to obstruction of the fallopian tubes?
The cause of this pathological condition is often a previous infectious disease. The doctor may recommend that the patient undergo appropriate tests in order to exclude the presence of an infectious pathology. If an infectious agent is detected, the doctor will offer the woman drug therapy aimed at eliminating it. At the next stage, the doctor may offer the patient reconstructive surgery on the fallopian tubes in order to restore their patency. Such an intervention is usually performed laparoscopically, but a complete cure is not always possible. If pregnancy does not occur after the operation, you will probably have to resort to IVF - a procedure for in vitro fertilization of an egg, which is subsequently “replanted” in the uterine cavity.
Treatment for infertility depends on the cause
Modern medicine has a significant arsenal of tools that can successfully combat female infertility. Therefore, if you are currently unable to get pregnant without treatment, do not despair! It is worth contacting a practicing gynecologist, a specialist in infertility, and most likely, the doctor will be able to choose the optimal treatment method for you, after which the long-awaited pregnancy will occur.
Infertility, to choose the right treatment. Many of the diagnoses are not as scary as they sound. Afterwards, the gynecologist will prescribe a treatment regimen for you, taking into account the individual characteristics of each woman. Including diagnosis, age of the patient and duration of infertility. After a course of treatment, if the woman is not pregnant within a reasonable time. It is worth taking tests again to confirm the diagnosis or change the treatment method.
Inflammation of the cervical canal caused by bacteria - treatment with antibiotics. Due to inflammation of the cervical mucus, sperm cannot enter the uterus to fertilize it. All treatments are aimed at restoring natural mucus. The easiest and fastest way is intrauterine insemination. When, during the period of ovulation, sperm are introduced through an intrauterine catheter directly to their destination, where they meet the egg. Using washed sperm, which increases the chance of fertilization several times, due to the absence of anti-sperm antibodies and unwanted cellular elements that do not have a beneficial effect on sperm activity.
Uterine infertility is combined with various factors and depends on a pronounced violation of the structure of the uterus:
- Unicornuate uterus. During pregnancy without complications, the woman may not be aware of her anomaly. In some cases, this disorder is directly related to kidney function. If you have any suspicions, undergo a kidney ultrasound and excretory urography to check the risk.
- A bicornuate uterus, in rare cases, causes problems during pregnancy. You should agree to surgery only in cases of extreme necessity, if the anomaly directly affects the process of conception or pregnancy.
- An arcuate uterus, in most cases, has nothing to do with infertility.
- A uterus with internal partitions, due to a possible violation of embryo implantation, is the basis for the inability to conceive or bear a child. Treatment with surgery has not been fully studied.
- Uterine (unions, Asherman's syndrome) treatment occurs by cutting out the adhesions, the name of the procedure is hysteroscopy. This procedure is used in the treatment of endometrial polyps, but in this case, it is also removed by curettage.
Treatment of fibroids or uterine fibroids can be done in two ways: surgical or conservative. With such a diagnosis, each case must be considered separately. This takes into account the patient’s age, the number of nodes, and the number of their locations. And only based on general data, a course of treatment is prescribed.

Photo: Method - intrauterine insemination
Treatment of tubal and peritoneal factors of infertility
Today, one of the types of treatment is microsurgical plastic surgery. With this type of intervention, complete restoration of tube patency is possible. But the chance of getting pregnant naturally is very small. It becomes approximately three
percent. Tubal infertility can be cured through the use of assisted reproductive technologies - fertilization.
Treatment of endometriosis
Depending on the patient’s age and severity, it occurs in four approaches:
- Waiting tactics, if this disease is in the primary stages, then the woman is constantly monitored to assess the extent of the disease.
- Surgical method. As a rule, this is a laparoscopic surgical intervention, which is used to remove visible foci of endometriosis and dissect adhesions. As a result, the natural structure of egg capture by the fallopian tube is restored.
- Medication method. Its basis is the use of hormones that block the growth of endometrioid lesions because the production of gonadtropins is reduced.
- A combined method, it includes a combination of two methods: medication and surgery. Of all the methods, it is the most effective, as it combines several options.
Treatment of ovarian (ovarian) factor infertility occurs with the help of diet and specially prescribed medications that restore the normal functioning of the hypothalamic-pituitary-ovarian axis. The drugs are selected individually, taking into account which of the functions fails.
Treatment of secondary amenorrhea in infertility occurs by normalizing the diet and eliminating non-sex hormones. If this course does not bring results, it is replaced with ovulation induction; this method has similarities in the treatment of ovarian (ovarian) factor. The choice is made on drugs that stimulate ovulation.
Is it possible to cure male infertility?
Just like in women, there are different forms of infertility. But among men, the most common spermograms are asthenozoospermia and oligozoospermia. How to cure male infertility in these cases and what does it affect? In the first case, this is a decrease in sperm motility, in the second, their number.
In case of oligozoospermia, intrauterine insemination with washed sperm is performed. When washing sperm, the number of active sperm can increase to two million. This is the minimum number at which successful fertilization can occur. The success of this procedure is that the sperm get immediately to the place where they can fertilize the egg. If after washing the sperm the number of active sperm is below normal. ICSI or IVF technologies will be required to help achieve the required level.
How to cure infertility in men diagnosed with... Or what is it? Lack of sperm in the ejaculate, or semen. Here it is necessary to eliminate the reason that causes the failure in the flow. Unfortunately, this can only be done through surgery. But in most cases it does not affect the result of the ejaculate. The most effective solution is testicular puncture. Subsequently, the sperm that have been extracted in this way, using intracytoplasmic injection into the egg, proceed to the fertilization process.
If, during the tests, a man has low testosterone, then first it is worth bringing this indicator back to normal. Stimulation of spermatogenesis using exogenous testosterones.
Modern methods of treating infertility
Take just one step and be in close proximity to your dreams. Innovations in medicine are relevant for every industry; many new and “old” types of diseases have become the reason for this. One of these troubles is the inability to have children. Overcoming infertility is the main task for fertility doctors. That is why modern science and medicine are constantly researching ways to prevent and treat childlessness and offer innovative treatment for male and female infertility.
Infertility treatment is a long and sometimes not very pleasant process. The primary task will be to determine the reasons for the inability to have children and its stage. A clinical examination, passing all the necessary tests and testing using ultrasound diagnostic tools will most likely help you learn much more about the disease and methods for overcoming it. Methods and methods for treating infertility are varied and directly depend on the degree of complexity of the disease.
Methods of treating infertility in medicine
In particularly difficult cases, when conceiving a baby naturally is problematic and infertility treatment does not bring the desired results, they resort to using the method of artificial insemination. Treatment of infertility in women using IVF (full name - in vitro fertilization) significantly increases the chances of getting pregnant. Successful use of this method contributes to a more “reliable” conception. The peculiarity is that this is “conception in vitro”, that is, the eggs are fertilized exclusively in the laboratory, and then the process of implantation into the uterus occurs.
The in vitro fertilization method is also often used as a treatment for infertility in men, affecting sperm motility and count.
The scheme for treating infertility with intrauterine insemination is simple: female eggs and male sperm are directly transferred to the natural place where the egg is fertilized, that is, directly into the fallopian tube. When the stage of the disease is quite complex, an already fertilized cell - an embryo - is transferred into the uterine tube. In 30% of cases this method gives a positive result. Before using the method, it is necessary to undergo diagnostic testing for patency of the fallopian tubes.
Another method used is insemination with male sperm. In other words, this is the preparation of previously taken male semen for enrichment in order to improve both the concentration and quality of sperm. The method is not particularly popular, since its effectiveness is only 15%, but it is still better than nothing.
Video: How to treat infertility
A long-awaited pregnancy can occur if you follow all doctors’ recommendations and apply effective infertility treatment. We should also not forget that infertility treatment is an integral part of the fight against childlessness. Traditional healing methods collected over the course of human existence can also help us look to the future with hope.
Is it possible to cure infertility with folk remedies? Each person makes his own choice. In any case, before starting treatment you need to know your diagnosis. You can try different methods:

- Many people know the healing power of sage; even in the Ancient East, women used it to conceive. They took a spoonful of herbs and brewed them with boiling water. They left it wrapped up for an hour and took a sip before each meal.
- In ancient Persia, if a woman could not get pregnant, she was treated with aloe leaves. The leaves were cut, crushed, and then poured with rendered goose fat and honey, the mixture was added to milk.
- In Ancient Rus', wormwood was used, and decoctions and tinctures were prepared.
- And in Ancient Greece, rhododendron was prepared as an alcoholic tincture, or brewed as tea.
Video: Infertility treatment. Grandmother's methods
Nowadays, in the arsenal of doctors dealing with infertility problems, there are many different methods of treating infertility. It is difficult to say which one is the best and most effective. In each specific situation, for each specific couple, an individual and most suitable method should be selected.
The foundation of infertility therapy is the elimination of the main cause that leads to reproductive dysfunction, as well as the treatment of concomitant pathologies. The approach should be comprehensive and aimed at restoring the integrity of the chain of all reproductive processes (ovulation, transfer of female and male reproductive cells, implantation of the egg into the uterine mucosa).
Also read this useful article -
Types of infertility treatment methods
Current methods of treating infertility are divided into two groups: methods that restore natural fertility, And assisted reproductive technologists And. Methods that restore natural fertility include laparoscopy, hysteroscopy and ovulation stimulation.
Laparoscopy
It is a minimally invasive surgical intervention using an optical system introduced through the anterior abdominal wall. With its help, it is possible to restore the patency of the fallopian tubes, remove adhesions, myomatous nodes, ovarian cysts and endometriotic lesions.
Hysteroscopy
is an endoscopic method that allows, with the help of special devices, to remove pathological formations in the uterus (intrauterine synechiae, submucous uterine fibroids, polyps, endometrial hyperplasia, uterine endometriosis, etc.). Hysteroscopy, like laparoscopy, is performed on an outpatient basis.
Classical ovulation stimulation
Ovulation stimulation used in cases where the cause of infertility is a pathological change in the menstrual cycle with a disruption in the process of the release of an egg from the ovary (ovulation). The method involves the introduction of a small amount of hormones into the female body, as a result of which the activity of the ovaries is normalized and, as a result, the egg fully matures. Subsequent conception occurs naturally.
If there is no result from using these conservative methods, they resort to assisted reproductive technologies (ART). These include artificial insemination with the sperm of the husband or donor, as well as in vitro fertilization procedures using ICSI, TESA and MESA methods.
Artificial insemination with husband's or donor's sperm
If a man has any spermogram abnormalities (a significant decrease in the number of sperm, their inferiority, disruption of their movement along the seminal ducts), the spouses may be offered therapy using artificial insemination method. This method is based on special processing of ejaculate (husband or donor) and its subsequent introduction into the uterine cavity.
In Vitro Fertilization (IVF)
E extracorporeal fertilization is the most effective method of overcoming infertility. Its principle is the fertilization of a woman’s reproductive cell (egg) outside her body and the subsequent transfer of the embryo into the uterine cavity. This method is indicated in cases of severe male infertility, immunological and combined infertility, as well as infertility of unknown origin.
ICSI method used in case of a sharp deterioration in sperm count and male infertility that cannot be corrected. ICSI involves the injection of a specially selected sperm directly into the egg. The procedure is performed using micromanipulation devices.
In the absence of male germ cells in the sperm (with azoospermia), they resort to puncture of the epididymis and testicle. The methods are called TESA and MESA. Thanks to them, doctors obtain sperm, after which ICSI is performed.
Donor programs
Donor programs are suitable for women who do not have a sexual partner or whose partner does not have sperm. In such a situation, the method of artificial insemination with donor sperm or IVF with donor sperm is used.
In case of early exhaustion in postmenopausal women, when the process of egg production stops due to age, donor eggs can be used to achieve pregnancy.
If it is impossible to carry a pregnancy to term, for example, in the absence of a uterus or in the presence of severe concomitant pathologies, you can resort to surrogacy. When carrying out such a program, embryos obtained as a result of the fusion of germ cells of genetic parents are transferred for further gestation into the uterine cavity of a surrogate mother.