Today, many people know what scoliosis is. This disease in Lately has become widespread throughout the world. Often, curvature of the cervical spine leads to disruption of the state of the body and the functioning of organs and systems.
The pathology can develop at any age; it provokes deformation of the spine and occurs in 45% of all diseases of the musculoskeletal system. Women develop scoliosis much more often than men. The reasons for its formation are ambiguous; presumably, the development of the disease may be influenced by trauma received in childhood.
Cervical scoliosis is a curvature of the spinal column vertical plane to the left or right side in its cervical region (from the first to the seventh vertebrae).
The disease is dangerous because it provokes a disruption of the blood supply to the brain due to compression of the artery.
The disease can appear at any age, most often it is observed in children who are over ten years old.
In medicine, scoliosis of the cervical spine can manifest itself in the following forms:
- Congenital scoliosis develops in prenatal period when part of the spine is not completely formed or appears sharp corner, which will progress as the child grows;
- Idiopathic curvature of the neck develops from birth until the child’s growth stops. This pathology appears for unknown reasons, which makes its treatment difficult;
- Neurogenic scoliosis appears as a result of impaired activity nervous system;
- Statistical scoliosis appears due to abnormal development of the limbs;
- Dysplastic scoliosis is characterized by lateral curvature of the spine due to metabolic disorders in its tissues and discs, as well as torsion.
The congenital form of the pathology is rare. In most cases, signs of the disease begin to appear during adolescence. In 80% of cases, the causes of scoliosis have no scientific explanation.
The disease has several degrees of severity:
- Scoliosis of the cervical spine of the 1st degree is characterized by a lowered position of the head and contracture of the shoulders due to curvature of the spine up to ten degrees;
- The second degree is determined by the presence of a curvature angle from ten to twenty-five degrees. In this case, there is torsion, an asymmetry of the neck line, which is visible in any position of the body;
- The third degree, in which the bending angle is from twenty-five to forty degrees. The person has severe torsion, muscle contracture, and all the signs that are inherent in the second degree of severity are also observed;
- Cervical scoliosis of the fourth degree of severity is characterized by a curvature of the spine of more than forty degrees. At this stage, the muscles in the pathological area are stretched, the symptoms of the disease intensify significantly, and disruption of the activity of the vascular and nervous systems appears.
Causes of neck scoliosis
There is no exact reason for the appearance of pathology in medicine. There are several theories according to which the disease may develop:
- Dysfunction of the endocrine gland is considered main reason the appearance of curvature of the spine in the neck area. During adolescence, hormonal changes in the body occur, which affects the development of the skeletal system, making it more plastic. Therefore, the spine can change under the influence of loads;
- Violation of the development of muscle tissue and ligaments with accelerated growth of the child. In this case, the ligaments and muscles become weak and cannot hold the spine in a certain shape;
- A change in bone tissue that leads to the development of dysplasia;
- Disruption of the nervous system, which leads to the appearance of syringomyelia and back deformity.
Neck scoliosis can also appear at birth due to intrauterine development disorders.

Today, children spend a lot of time sitting in front of a PC monitor; they practically do not engage in physical activity. This can cause curvature of the spine in the cervical region.
Symptoms and signs of scoliosis development
Curvature of the cervical vertebrae disrupts the composition and structure of the spine, which leads to its deformation and disruption of the functioning of organs and systems. In the first two stages of the pathology, there are no symptoms of the disease, the patient does not make any complaints.
At the third stage of development of the disease, an asymmetry in the position of the head and the contour of the shoulders is observed, and one can see that a person’s ears are at different distances relative to the horizontal line. In severe cases, cervical scoliosis manifests symptoms in the form of impaired formation of the skull bones. These phenomena are accompanied by headaches, weakness and dizziness, the development of insomnia, memory impairment and retardation of consciousness.
Nerve reflexes weaken over time, neck pain appears, which becomes stronger when coughing or sneezing, the occipital muscles are in constant voltage, the limb on the side of the curvature becomes numb. When the bones of the skull are deformed, thoracic scoliosis can develop.
Symptoms of the pathology appear in the last two stages of the disease, so it is important to diagnose it at initial stage development to avoid negative consequences in the future.
Curvature of the spine in the cervical region can lead to disability, the development of paresis or paralysis of the limbs. This often occurs due to compression of the blood vessels and nerves in the spine. This pathology must be treated, as it does not go away on its own.
Diagnostic measures
Before correcting the curvature of the cervical spine, the doctor must make a diagnosis. Diagnosis of the disease begins with a history and examination of the patient. To determine the curvature of the spine, the patient needs to lean forward with his arms down.
The doctor examines the line of the vertebrae, the asymmetry of the body and the presence of curvature. To make an accurate diagnosis, radiography is prescribed. This method also allows you to identify the degree of curvature angle to determine the stage of development of the pathology.
Often, the doctor prescribes CT and MRI to study the problem in more detail. Additional research methods are used to determine the extent of damage to internal organs, blood vessels and nerves.
Treatment of pathology
Treatment of cervical scoliosis involves complex treatment. The choice of treatment method depends on the degree of damage to the spine, the form of the disease and general condition body.
Conservative treatment is aimed at correcting posture, stopping the pathological process in order to prevent the use of surgical intervention. For this purpose, various techniques are used:
- Manual therapy is used for relief pain, restoration of the shape of the spine;
- Acupuncture to stop the inflammatory process;
- Massage to normalize blood circulation, relieve swelling and improve metabolism;
- Tszyu therapy is used to normalize blood flow and tissue nutrition, as well as to supply oxygen to the brain;
- PRP therapy is modern method, designed to activate the processes of bone tissue regeneration, restore the activity of organs and the musculoskeletal system;
- Electrical stimulation of muscle tissue in the affected area.

The doctor also prescribes wearing a corset, proper nutrition and sleeping on a hard mattress, exercise therapy and gymnastics, as well as hardening.
Medicines are not used in the treatment of spinal curvature. The doctor can only prescribe painkillers to relieve pain, as well as calcium and phosphorus.
In some cases, scoliosis of the cervical spine is treated surgically. The operation is performed in the absence of effect from conservative therapy, as well as in advanced forms of the disease and in the presence of severe unbearable pain. In this case, the following methods can be used:
- Surgery to stop the growth of the vertebrae, in which the plate and disc are removed from the side that protrudes;
- Stopping spinal curvature. To do this, a bone graft is used, which is placed between the vertebrae to immobilize them;
- Surgery to eliminate a cosmetic defect.
In some cases, surgery can provoke the development of serious complications in the form of disruption of the vascular system, damage to the spinal cord, destruction of the vertebrae, and the development of purulent inflammation.
After surgery, it takes three months for the bones to heal. The doctor prescribes a plaster cast and wearing a corset to support and strengthen the back. After five weeks, the patient must visit a rheumatologist for joint sessions to restore the spine. These classes usually take place three times a week for two months. After rehabilitation, the patient must limit physical activity for the rest of his life.

Scoliosis of the cervical spine can be treated in many ways, but it is best done on early stage development of the disease or prevent its occurrence altogether.
Prognosis and prevention
The prognosis of the pathology is most often favorable. In severe cases, disability may develop.
Curvature of the neck, or torticollis, is manifested by tilting the head and turning it to the side. This condition occurs due to pathology of the bones of the cervical spine, neuralgia or soft tissue damage.
The curvature can be acquired or congenital. This condition is extremely dangerous, as it leads to deformations of the skull bones and disruption of the central nervous system. In other words, curvature of the neck spine is the cause of dementia, developmental delays, memory impairment, vision, hearing and other conditions. Therapy for the disease depends on the causes that caused it, the patient’s age, his general condition and other factors.
Torticollis in children
Curvature of the neck in a child most often begins during intrauterine development.
The reasons may be infectious diseases suffered by the mother, the position of the child’s body in the uterus, or abnormalities in the pelvic bones of a pregnant woman. It happens that the curvature is a consequence of a chromosomal mutation. Types of disease:
- Neck curvature of idiopathic origin. The very name of the pathology suggests that the cause of its occurrence is unknown. The truth and force of the curvature is extremely small and the position of the head is not fixed. There is a hypothesis that such an influence is a consequence of the position of the body in the womb. However, this form can also have obvious complications, for example, perinatal encephalopathy.
- If a child’s sternocleidomastoid muscle becomes thicker or shortened during its formation, he may develop myogenic torticollis. The reason for this situation with the neck is usually the long-term position of the child across, that is, his head was pressed against the pelvic bones for a long time. With this pathology, the child’s head remains motionless, as the muscles become denser and cause pain when moving. In the future, he may develop scoliosis of the spine, the skull is curved, the eyes occupy different heights on it, and brain function is disrupted.
- Curvature of the neck in infants can be a consequence of underdevelopment of the cervical vertebrae or their fusion into one bone. This phenomenon is called osteogenic pathology. The head is set very low on the shoulders and loses the ability to turn. Usually the pathology is not limited to the cervical region; most often the lumbar region also loses mobility.
- With the neurogenic component of the pathology, not only the neck is turned to one side, but also half of the entire body (leg and arm are bent) is skewed to one side. In general, the child can move, but at rest the muscles return to their usual position and the curvature returns.
- With arthrogenic torticollis, there is a congenital defect of the cervical vertebra, namely its rotational dislocation.
Torticollis in adults

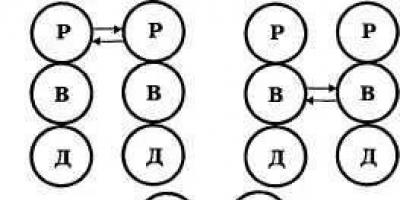
Neck strain can occur at any age. It is usually caused by physical trauma. Such damage to the cervical vertebrae is also called acquired, because it can occur in infancy, for example, on the first day of life as a result of a birth injury, for example, when strangulated by the umbilical cord. As a child matures, he may become a victim of infection or cold, which also leads to curvature. Possible positions of neck curvature in adults are shown in the photo below.

The causes of curvature of the cervical vertebrae may lie in the following:
- A child acquires installation torticollis when the head is positioned in a crib for a long time in an uncomfortable manner. No soft tissue or bone pathologies are observed in this case.
- Reflex curvature of the neck becomes a consequence of various pathologies, for example, otitis media or ear inflammation. They cause severe pain, which forces a person to involuntarily bend his head towards the affected ear. Also, involuntary curvature is caused by purulent abscesses in the neck due to mastoiditis and other similar diseases.
- With a compensatory curvature of the neck, the patient tries by turning his head to compensate for the absence of an eye, strabismus, labyrinthitis (a disease inner ear). This half-rotation allows you to increase your visibility or reduce dizziness.
- In case of traumatic injury to the neck, we are usually talking about a fracture. This phenomenon is extremely painful for the patient. Not only the position of the head causes pain, but also an elementary attempt to touch the injured area. Such an injury may not be accompanied by a vertebral fracture, that is, it may be the result of a dislocation, but the symptoms remain the same: severe pain and inability to move.
- Several factors can lead to the traumatic phase at once. infectious diseases: syphilis, osteomyelitis. All this can easily lead to a fracture and curvature of the neck.
- Torticollis can be a consequence of myositis, muscle inflammation, as well as inflammatory processes in the lymph nodes of the neck, in its ligaments and soft tissues, chest and spine.
Diagnosis of pathology

How to correct a curvature of the neck is decided by the doctor only after an accurate diagnosis. One glance at the patient is not enough for diagnosis, although the curvature looks quite characteristic. In order to understand why the child’s neck is crooked, the doctor interviews the mother about how the pregnancy and childbirth proceeded. Were there any abnormalities recorded in hormone tests? It also matters how the baby was born (already with a curvature or it occurred later). The patient must be examined by a neurologist.
For an accurate diagnosis, modern instrumental methods, computed tomography or magnetic resonance imaging are used. If this is not possible, then a method such as radiography is fully justified.
We should not forget that in case of associated diseases it will be necessary to consult with specialized specialists, for example, for strabismus you should visit an ophthalmologist, for syphilis - a venereologist, sometimes even a psychiatrist may be needed.
Treatment of pathology

Treatment for curvature of the neck is very diverse; the choice of method depends on the type and severity of the pathology. Sometimes conservative or physiotherapeutic treatment is sufficient, and sometimes surgery cannot be avoided.
Physiotherapy includes electrophoresis using various drugs (lidase, potassium iodide). Irradiation of the affected area of the neck with ultraviolet rays helps. Most often, therapeutic massage is used, especially for newborn patients.
The patient also takes a number of medications various actions. The treatment regimen includes pain medications, antibiotics, muscle relaxants, or anticonvulsants.
Typically, treatment using these methods takes at least 6 months, provided they are carried out regularly and correctly.
If such treatment is ineffective or injury occurs, surgery is performed. It can affect muscles, ligaments and even bones.
After the operation, the patient must wear a special neck corset for some time, holding the cervical vertebrae in place. correct position.
Therapeutic gymnastics and position
For young children, the most effective and painless method of treatment is gymnastics. It is useful not only for the neck, but also for the entire developing body. It’s easy to do; anyone can do it after a few sessions with a physiotherapist.

To stretch the neck muscles, you need to place the baby on the table so that his head hangs over the edge. Under no circumstances should you let her out of your hands. You need to very slowly and gradually lower your hands with the baby’s head to the edge of the table, and over time, beyond its edge. This way the muscles will gradually stretch without tearing or injury.
For the same purpose - stretching the muscles, you need to turn the baby's head in one direction or the other while lying down. Muscle stretching can also be done in a vertical position, holding the baby in your arms and holding his head.
Forecast

In general, the prognosis for neck curvature is positive. Timely therapy, even if it is a surgical operation, restores the cervical vertebrae and soft tissues in full. The only exception is Klippel-Feil syndrome, in which the bones of the cervical spine turn into a monolith.
Consequences
If a curvature of the neck is left without timely treatment, a person may develop dangerous conditions, sometimes incompatible with life.
In addition to the visually unaesthetic appearance, which in itself causes psychological trauma in the child, systemic disorders may also occur. For example, mental retardation, visual impairment, hearing impairment, pathology of the musculoskeletal system. And if the patient experiences compression of the trachea, then pulmonary failure and general oxygen starvation develop.
Prevention
To prevent congenital curvature of the neck, the expectant mother must follow preventive measures. She should be observed by a local doctor throughout her pregnancy, undergo tests and undergo all necessary procedures. In this case, it will be possible to diagnose the pathology at the very beginning and easily cure it. During pregnancy, you should not eat foods containing preservatives and dyes. You should not smoke or drink alcohol.
To prevent injuries that cause neck curvature, it is necessary to follow safety precautions at work and in sports, and in case of injuries, immediately consult a doctor.
Orthopedics
A separate topic of prevention is orthopedics. Not only the condition of the neck, but also the entire body depends on how the head lies during sleep. Therefore, the pillow should not be hard or soft, the head should rise 5-7 cm above the mattress. Canvas bags with salt or buckwheat husks are excellent for newborns. Pillowcases should be made of fabric that easily absorbs sweat.

Conclusion
Neck curvature cannot be left without treatment, because the pathology is fraught with serious consequences, sometimes irreversible. At the first signs of illness, you should immediately consult a doctor. In most cases, the prognosis is favorable.
The configuration of the neck changes with enlargement of the lymph nodes, salivary glands, tumors of soft tissues, nerves, spine, carotid, thyroid glands, aberrantly located goiter, diverticula of the pharynx and esophagus, aneurysms of the neck vessels, subcutaneous emphysema, hematomas, abscesses and phlegmon, developmental anomalies, mediastinal tumors.
A peculiar deformation - a thick neck with a cone downwards (Manuylov's symptom) - is observed in the cervical ribs.
Neck deformity and pain occur due to inflammation of the salivary glands - sialoddenosis. Outwardly, it resembles the swollen cheeks of a hamster.
Neck deformity occurs with systemic enlargement of the salivary and lymphatic glands and is accompanied by a decrease in salivation. Splenomegaly is characteristic.
Shortening of the neck (“a person without a neck”) and restriction of movements occur when underdeveloped vertebrae are fused (Klippel-Feil syndrome), as well as during normal synostosis. In the first case, there is also a downward shift in the hair growth boundary.
“Barbarian posture” is characteristic of osteochondrosis and injury to the spinous processes. Fixation of the neck in an abducted position occurs when torticollis (congenital or acquired deformity) associated with fibrosis or shortening of the sternocleidomastoid muscle.
A typical congenital deformity is also the pterygoid neck - the formation of triangular sail-like folds on its lateral surfaces. Wing-shaped folds of skin in the neck area are combined with the same folds in the joint area, swelling of the extremities, and other developmental defects.
Symmetrical enlargement of the neck occurs with systemic tumor damage to the salivary glands, diffuse disease of the thyroid gland, lymph nodes (lymphosarcoma, lymphogranulomatosis, sarcoidosis, blood diseases), subcutaneous emphysema, myxedema, obesity. The accumulation of lymph nodes deforms the neck either at the root, or in the submandibular, parotid areas, along the sternocleidomastoid muscle. Palpation examination reveals all the characteristic signs of altered lymph nodes. Smoothing of the typical contours of the neck in the median triangle also occurs with diffuse enlargement of the thyroid gland.
Subcutaneous emphysema leads to expansion of the contours of the neck, mainly at the base and is often combined with mediastinal emphysema, and crepitus on palpation is characteristic; a history can reveal a previous injury or an endoscopic examination.
Asymmetrical deformities of the neck are formed due to nodular goiter, pathology of the lymph nodes, aneurysms, tumors and cysts. Pulsation is often visible - direct in aneurysms, transmitted - in tumors and diseases of the lymph nodes. The disappearance of pulsation of the artery under the tumor is a sign of its malignancy. Tumor-like deformity of the neck most often occurs when the lymph nodes are enlarged with characteristic swelling in the projection of the lymphatic collectors of the neck.
Limited deformations along the sternocleidomastoid muscle occur with aberrantly located goiter, aneurysms of the neck vessels, and tumors of the carotid gland. Carotid tumors do not move vertically, and blood pressure often increases after palpation.
Clear, round formations in the area of the hyoid bone, as a rule, turn out to be median cysts. If the cyst is small, it is slightly displaced from the hyoid bone; when you tilt your head back, you can see a cord running from the cyst to the bone. Pulsatile formations are usually aneurysms. Patients experience noise in the head and throbbing pain.
Behind the vertical branch of the lower jaw, tumor-like deformities occur due to a tumor, less often a cyst, or inflammation of the parotid salivary gland. Chronic deformities are usually caused by a tumor, acute deformities are caused by mumps. The neck is asymmetrically deformed in the upper half and with woody phlegmon of Chasignac, which is accompanied by severe pain, dysphagia, intoxication, the skin is hyperemic, with a cyanotic tint.
Scoliosis is a deformation of the spine in several planes around its axis. It occurs in any part of the spine: from the lumbar to the cervicothoracic.
Curvature of the cervical spine is also called “high scoliosis.” This disease is much more common in women; it occurs in them 3 times more often than in men. It occurs in childhood. Therefore, parents should think about correct positioning diagnosis and treatment as early as possible.
This will help your child avoid neck and back problems in adulthood.
However, if a curvature is already present in an adult, this does not mean that treatment is already late: correction of posture and head position should begin at any age, when problems have arisen with this and a final diagnosis has been established.
To prevent and treat JOINT DISEASES, our regular reader uses the increasingly popular NON-SURGERY treatment method recommended by leading German and Israeli orthopedists. After carefully reviewing it, we decided to offer it to your attention.
Causes of curvature in the cervical spine
There are two types of scoliosis: congenital and acquired. Congenital – associated with birth injuries and requires a special approach to treatment depending on the nature of the injury.
Acquired curvature does not have any one specific cause. As a rule, it is caused by a complex of several factors. Therefore, there are several medical theories about why it occurs:

The severity of the disease also varies in the number of arcs of curvature (from one arc to three) and in severity (from the first to fourth stages):
- the first – from 1 to 10 degrees;
- the second - from 11 to 25 degrees;
- third - from 26 to 40 degrees;
- fourth - more than 40 degrees.
Symptoms of cervical scoliosis
 Symptoms of curvature are divided into general and specific (characteristic only for this pathology).
Symptoms of curvature are divided into general and specific (characteristic only for this pathology).
In the first two stages of the disease there are still no particularly striking manifestations. However, in the third and fourth stages, the severity of the spinal deformity can already be seen with the naked eye. It is characterized by asymmetry in the position of the head; it can be tilted forward or to one side, right or left, sometimes you can see that the patient’s ears are at different heights relative to each other. The violation of the symmetry of the contour of the shoulders is also very noticeable; at the last stage, changes in the symmetry of the pelvis are already visible. In some cases, if left untreated, abnormal development of the skull bones becomes visible. All these symptoms are a reason to immediately consult a doctor and begin treatment.

Most patients, as a rule, complain of difficulties in movement, pain when turning or tilting their head. Some patients come to the doctor with complaints solely about the aesthetic effects of the curvature, especially in the initial stages of the disease.
Common symptoms include headaches, fatigue and general weakness. The patient may also experience dizziness, especially when trying to tilt the head sharply. All this occurs due to compression of blood vessels and, as a result, circulatory disorders, including in the brain.
Often, with the first or second degree of cervical curvature, a person does not pay attention to the problems. As a rule, all symptoms are attributed to fatigue or overexertion. But if a person complains of both a headache and neck pain at the same time, then this is a clear sign of the onset of serious problems.
In some countries, the first stage of scoliosis is not considered a disease at all and does not require any intervention from doctors. However, despite this, you should be aware of it and take measures to maintain this department in a healthy state. After all, the very fact of a small anomaly already indicates an increased risk and the possibility of deterioration.
Diagnosis of the disease

A doctor can accurately determine the degree of scoliosis and its type based on both a visual examination and after studying the patient’s X-rays. You should not engage in self-diagnosis: determining the curvature of the spine is the field of activity only of orthopedic doctors, and independent intervention can result in a worsening of the condition, or even serious consequences for the patient.
The main method of visual diagnosis is as follows: the patient is asked to lean forward and lower his arms. In this position, the doctor will clearly notice the deformation of the spine and the displacement of individual vertebrae relative to each other.
But the main method for diagnosing curvature in the spine, especially in its cervical region, is an X-ray examination. The image allows you to accurately determine the angle of curvature, its degree, and sometimes find out the cause of the deformation. This is done by calculating the Cobb angle. To measure it, it is necessary to draw two straight lines parallel to the neutral vertebrae on the anteroposterior projection x-ray and where they intersect, this angle is measured. Using these data, you can judge the severity of back and neck problems.
If these techniques are not enough, the doctor may additionally prescribe an MRI of the spine.
Treatment

Treatment very much depends on factors such as the severity of the disease, its form, the rate of progression and, of course, the patient’s health at the time of treatment. Therefore, when a doctor makes such a diagnosis, it is better not to put off starting to solve the problem, but to get down to business even before the pathology reaches some serious stage and complicates treatment.
The so-called folk remedies, breathing exercises, massage using any special techniques and psychotherapeutic practices using proprietary methods, but their effectiveness has not yet been confirmed by research.
Of the practice-proven methods of treatment, there are two: conservative and surgical.
Conservative
This method of treatment is carried out by the patient at home, but under the supervision of a doctor. Basically it consists of compliance correct posture and performing a set of specific exercises to increase muscle support for the neck and straighten the cervical part. Conservative therapy includes the following health measures:
- physiotherapy;
- classes in the pool;
- proper organization of the workplace and sleeping on a hard bed;
- massage: therapeutic and manual;
- electrical stimulation of muscles;
- wearing a corset.

Outside of sleep, you need to carefully maintain your posture ordinary life, avoid positions that put pressure on the cervical vertebrae, keep your head straight. The child should be placed on a chair that matches the height of the table.
The next step is physical therapy. The patient needs to learn a set of special exercises for cervical scoliosis and perform them regularly. It will be very useful to combine physical education with swimming lessons.
The doctor may also prescribe restorative therapeutic massage and electrical stimulation. This will help improve spinal support by activating muscle function.
Particular attention should be paid to nutrition. If scoliosis is caused by softening of the bones due to a lack of minerals and trace elements, then an increase in foods with a high content of calcium and phosphorus in the diet will significantly slow down its development.
The last thing worth noting is the use of special orthopedic corsets for the upper back and other supporting devices (including for the neck in case of a serious stage of deformity). They allow a person to straighten the cervical spine, ensure that the neck is fixed in the correct position and receive a slight massage effect.
But you need to know that support devices lead to weakening of muscles and a decrease in their motor activity, which is very bad for scoliotic neck disease. It is important to know that corsets and support devices cannot be used without consulting an orthopedic doctor; this is a rather radical means of correction. To a greater extent, this applies to rigid structures, which, in addition to doctor’s prescriptions, also require adherence to a wearing regime (no more than a few hours a day), since the consequences of abuse can be intervertebral hernia.
Operative or surgical method

Involved in treatment only if conservative therapy does not produce significant results. Most often, indications for surgical treatment appear already at the last, fourth stage of scoliosis.
Any surgical intervention requires careful monitoring of the patient’s condition and careful selection of a technique by which the condition of the spine will be improved.
Surgical treatment has several options. Their choice depends on the type of pathology that needs to be eliminated:
- limiting the asymmetry of vertebral growth (this is resection from the convex side of a part of the intervertebral disc, which complicates the progression of curvature);
- stabilization of spinal deformity (spinal fusion or fusion of several adjacent vertebrae in order to immobilize them, the use of a bone graft, which allows stopping the movement of the vertebrae and preventing the increase in pathology);
- correction of curvature - carried out using a rigid frame installed directly on the deformed area;
- operations of a cosmetic nature - do not eliminate the disease, but relieve some of its defects.
U surgical methods treatment has a lot of negative effects. In particular, in particularly difficult cases, complete immobility of the vertebrae may occur, and the most disastrous result can be the threat of their complete fusion. Unfortunately, when fusion occurs, the patient becomes disabled and this cannot be corrected in any way.
Therefore, surgery is carried out with caution and only on the condition that no other methods stop the deterioration of the condition. If the patient has not yet used all the chances to correct his position without resorting to them, then the doctor should make every effort to eliminate the problem in a conservative way.
Prevention
Prevention of cervical scoliosis should begin in early childhood. Physical therapy, body position control, load distribution, a course of specialized massage - all this will help smooth out the negative effects of curvature, even if the child has a predisposition to it. You should especially seriously combat a sedentary lifestyle, because it can lead to weakening of muscles and the development of disease.

Consequences of scoliosis
Scoliosis is a disease whose consequences are significantly extended over time. This means that complications themselves can appear at any time. This should be taken into account and not delay visiting an orthopedist.
The most common complications of curvature:
- Problems with the musculoskeletal system, stiff movements and muscle pain.
- Circulatory disorders. Incorrect positioning of the spine in space can negatively affect the functioning of blood vessels.
- Headache. It is the most common symptom and complication of cervical scoliosis and reduces the patient’s quality of life.
Of course, it is best not to let the consequences of the curvature manifest itself and contact specialists for treatment in a timely manner.
Cervical scoliosis is a very common disease of our time. A sedentary life, sleeping on too soft surfaces, lack of positive stress on the back muscles - this only contributes to the appearance of diseases and disorders in the spine, and in its cervical part, in particular. Cervical scoliosis can not only look unsightly, but also causes a lot of unpleasant problems for a person: headaches, dizziness, and sometimes hypoxia (lack of oxygen) in the brain. This is an extremely powerful argument in favor of preventing its development. Because treatment will cost more and take much longer than prevention.
NECK DEFORMATIONS Congenital muscular torticollis Torticollis is a deformity of the neck of congenital or acquired origin, characterized by an incorrect position of the head - tilting to the side and turning it. Torticollis occurs most often as a result of pathological changes in soft tissues, mainly in the sternocleidomastoid muscle (m. sternocleido-mastoidcus), less often as a result of anomalies in the development of the cervical spine. Based on the pathogenesis of suffering, they distinguish between mpogenic, os-sebaceous, neurogenic, dermo-desmogenic and compensatory forms. Congenital muscular torticollis, according to most researchers, in relation to other congenital diseases of the musculoskeletal system ranges from 5 to 12% (S. T. Zatsepin), ranking third in frequency after congenital clubfoot and congenital hip dislocation. According to a number of authors (S. T. Zatsepin, M. O. Frpdlyand), this deformity occurs mainly in girls and is more often right-sided. Congenital muscular torticollis can also be bilateral. Among the symptoms of this disease, one should note the limitation of tilting the head in the opposite direction due to shortening of the sternocleidomastial muscle. Ethnology and pathogenesis. The cause and development of suffering remain not fully understood at the present time. All existing theories cannot fully explain the diversity of the clinical picture and the essence of the pathological process. For many years, the prevailing opinion was that muscular torticollis was caused by abnormal fetal position. It was only in 1838 that Stroeckmeier first suggested that muscular torticollis occurs as a result of damage to the sternocleidomastial muscle at the time of childbirth, and the resulting hematoma and its subsequent scarring lead to shortening of this muscle. Traumatic theory of origin muscular torticollis found many supporters. Thus, according to S. A. Novotelyyuva, birth trauma leads not only to shortening of the sternocleidomastillary muscle, but also to a reflex disturbance of its trophism, resulting in shrinkage of the muscle. However, further observations by a number of researchers did not confirm the traumatic theory of the occurrence of muscular torticollis; it was not possible to obtain blood during puncture of the changed part of the sternocleidomastillary muscle and during its histological examination. A. V. Protasevich (1934) cut this muscle in 2-week-old rabbits, but its growth was not impaired in the future. Peterson believed that as a result of incorrect position of the fetus in the uterine cavity, persistent shortening of the sternocleidomastial muscle occurs, which complicates childbirth and often leads to damage to this muscle. In 1895, Mikulich first put forward the inflammatory theory of muscular torticollis. The author believed that as a result of penetration of microbes into the sternocleidomastillary muscle of the fetus, chronic interstitial palpable myositis occurs, leading to the development of the indicated deformity. In 1902, Felker suggested that muscular torticollis is a consequence of ischemia. Ischemic contracture of the sternocleidomastial muscle, from his point of view, is the result of pressure from the fetal shoulder on the upper part of the neck, which can lead to compression of this muscle in its lower part, which, according to the author, does not have its own vessels and is supplied blood from the upper half. At the same time, the pectoral clavicular-mamillary muscle is supplied with blood from a large number of arterial branches that have numerous anastomoses; even in the changed part of this muscle, it is possible to detect unchanged vessels with preserved conductivity. In this regard, without completely rejecting the assumption about the possibility of impaired blood supply to the sternocleidomastial muscle during childbirth, muscle ischemia cannot be considered the only cause of muscular torticollis, which is confirmed by a number of histological studies. From our point of view, which coincides with the opinion of II. N. Aleksinsky (1896), V. M. Afanasyeva (1944) and S. T. Zatsepin (1960), it is most correct to assume that congenital muscular torticollis occurs as a result of a congenital malformation of the sternocleidomastial muscle. Trauma, which is often observed during childbirth, especially with the buttock position, only seems to aggravate the deformity. The degree of severity of suffering is directly dependent on the severity of underdevelopment of muscle fibers and the degree of replacement of muscle tissue with connective tissue. Therefore, only those children who have a significant or significant number of underdeveloped muscle fibers are born with clinically pronounced symptoms of congenital muscular torticollis. most of muscles are replaced by fibrous connective tissue. This is confirmed by the observations of Kostendieck, who noted clinical underdevelopment of the sternocleidomastial muscle in 2.6% of newborns in the absence of pronounced symptoms of torticollis. Clinic. The picture of congenital muscular torticollis is extremely diverse and mainly depends on the age of the child. As a rule, in the first 7-10 days of a patient’s life, underdevelopment of the sternocleidomastial muscle can be detected in only some of them. Thus, S. T. Zatsepin found congenital muscular torticollis in only 29 of 649 examined newborns. Only in the 2-3rd week of a child’s life does the affected sternocleidomastial muscle undergo significant changes - it thickens in the middle or lower -in its middle part, thickens and shortens, as a result of which a swelling of dense consistency appears on the corresponding half of the neck, not fused with the underlying soft tissues . When a dense cord appears, a tilt of the head occurs, and later an asymmetry in the size and location of the ears occurs. With age, in most children, the compaction in the area of the sternocleidomastial muscle significantly decreases or completely disappears. In a minority of cases, the compaction and thickening of this muscle gradually increases, it becomes less elastic, extensible and shortens. The tilt of the head and its rotation increase, its mobility is limited, facial asymmetry becomes more noticeable, and skull asymmetry appears. The most pronounced deformity is in congenital muscular torticollis at 3-6 years of age. Its severity is caused mainly by a lag in the growth of the sternocleidomastial muscle with the correct growth of the cervical spine. A clinical examination of a sick child from the front reveals a sharp asymmetry of the face and skull. The head is tilted forward and towards the changed sternocleidomastoid muscle, but turned in the opposite direction. The higher position of the shoulder girdle and scapula on the eastern side is marked. When examining the patient from behind, asymmetry of the neck, tilt of the head, and higher position of the scapula are noticeable. In most patients, both legs of the sternocleidomastial muscle are altered, and only in some of them is one. The affected sternocleidomastial muscle is usually thinner than normal and has the shape of a cord that is dense to the touch. As a rule, the trapezius and serratus anterior muscles are shortened on the affected side, which leads to an asymmetrical position of the shoulder girdle and scapula. According to S. T. Zatsepin, the tension of the affected sternocleidomastoid muscle is not associated with its tonic contraction, but with the pull of the opposite healthy muscle, trying to align the position of the head. The degree of shortening of the sternocleidomastial muscle depends mainly on the magnitude of the discrepancy in its length and the cervical spine; the severity of the tilt and rotation of the head is due to changes in the corresponding pedicle of this muscle. Thus, when the thoracic pedicle is predominantly affected, the rotation of the thoracic pedicle is more pronounced, and when there are gross changes in the clavicular pedicle, its inclination is more pronounced. Tension of the sternocleidomastoid muscle and tilt of the spine lead to changes in the cervical and thoracic spine. Lorenz divides them into two types. With a mildly expressed deformity, simple kyphosis is observed in the cervical spine, convexly facing in the direction opposite to the deformity. In more severe forms of suffering and in older children, as a rule, S-shaped scoliosis of the cervical, thoracic and lumbar spine is detected. The traction of the sternocleidomastial muscle affects the shape of the repair and mastoid process, which in patients with congenital muscular torticollis is enlarged, and the cells of its air cavity are larger. As a rule, the direction of the ear canal changes. The half of the head on the modified side becomes more flattened and wider. The eyes and eyebrows on the affected side are located lower than on the healthy side. There is abnormal development of the upper and lower jaws, as well as the paranasal cavities, nasal septum, and hard palate. Concomitant symptoms with congenital muscular torticollis are limitation of visual fields. X-rays with congenital muscular torticollis do not reveal any other changes other than the symmetry of the skull. Shortening of both sternocleidomastial muscles is extremely rare. In this case, the child’s head is tilted or backward so that the back of the head approaches the back, and the face looks up or forward. This deformity occurs in cases where the length of the sternocleidomastial muscles does not correspond so much to the length of the cervical spine that the patient is unable to tilt his head either forward or backward. As a rule, in such patients the range of head movement is sharply limited, mainly in the sagittal plane, and the cervical spine is significantly shortened. Differential d and diagnostics. Recognizing congenital muscular torticollis in the first year of a child’s life does not present significant difficulties, . since acquired forms of deformation are extremely rare in them. In older children, congenital muscular torticollis must be differentiated from Klippel-Feil syndrome, cervical ribs, wedge-shaped hemivertebrae of the neck, pterygoid neck, as well as acquired forms of torticollis—Grisel’s disease (see below), spastic, dermatogeal and desmagnetic forms of torticollis. Spasmodic torticollis is one of the types of hyperkinesis and is characterized by movements that do not obey the will of the patient, or a forced position of the head due to the alternation of clopic and tonic spasms of the neck muscles. Suffering occurs after encephalitis, develops gradually and progresses tirelessly over time. Dermatologic forms of torticollis are caused by the presence of extensive scars in the neck area after a burn or lupus. Desmogenic forms of torticollis are the result of cervical lymphadenitis or phlegmon. Torticollis due to chronic inflammatory processes in the sternocleidomastial muscle: is the result of myositis, typhus, malaria, scarlet fever, gummous syphilis. An inclined position of the head is possible as a consequence of injury or a pathological process in the bodies of the cervical vertebrae - osteomyelitis, tuberculosis, actinomycosis, neoplasms. Treatment. Conservative treatment of muscular torticollis should begin at 2 weeks of age. Basically, it consists of corrective gymnastic exercises performed 3-4 times a day for 5-10 minutes. In this case, the head of the child lying on his back is clasped with both hands and given the correct position as possible, that is, tilted in the direction opposite to the affected muscle and turned to the healthy one. The described manipulation is so simple that it can be successfully performed by the mother. Therapeutic gymnastics should be carried out without violence, since as a result of excessive stretching of the sternocleidomastial muscle, even more profound changes can occur. At the same time, a massage of the healthy sternocleidomastial muscle and kneading of the injured one, as well as a course of physiotherapeutic procedures (UHF), are prescribed. In children aged 6-8 weeks, in order to prevent scarring of the affected muscle, a course of ion-galvanization with potassium iodide, consisting of 30 sessions, can be carried out; the course of treatment can be repeated after 3-4 months. During this period, great importance should be attached to massage of the entire half of the face and neck on the sore side. To hold the child's head in the achieved position of hypercorrection, it is recommended to wear a cardboard-wadding Shants collar or a cap attached with ribbons on the sore side to a fabric bra. You can place the child in a specially made plaster crib or fix the head in the correct position between the bags with sand. A newborn's crib indoors should be installed in such a way that the healthy half of the neck faces the wall. By watching what is happening in the room and turning his head towards the changed muscle, the child will involuntarily give it the correct position. With a mild form of muscular torticollis, timely conservative treatment leads to a complete cure of the child in the first year of his life. With a more severe degree of deformity, conservative treatment should be continued until the age of 3, when the symptoms of increased volume and thickening of the sternocleidomastial muscle completely disappear. In some patients with significant underdevelopment of the sternocleidomastial muscle, elimination of the deformity is only possible through surgery. Surgical treatment of congenital muscular torticollis in order to eliminate the main symptoms of the deformity is indicated for children 3-4 years old or for those older patients in whom conservative treatment did not lead to stabilization of the pathological process. The indication for surgery is increasing asymmetry of the face and skull, the development of which, unlike the symptoms of mouse tension and head tilt, cannot be prevented by conservative methods.